I often find it frustrating that here I am, a life long asthmatic, a Respiratory therapist and an asthma educator, yet still unable in normal conversation, to describe what makes my type of asthma so different from others. When asked to define asthma in general, I usually give the spiel about how asthma is an inflammatory disease of the airways, and blah.. blah.. blah .
But lately it’s hit me that the explanation Ive been giving for so long, though medically correct and easier for lay people to understand, doesn’t really paint an accurate picture of what’s actually happening with MY own asthma. So, I’d like to take this opportunity to explain more in depth why my type of asthma is so different. I hope I can do this without boring you, or worse, loosing you.
What makes my asthma so different from others, is that are actually TWO distinct processes going on in my lungs. A “double whammy” if you will. Both of these components are related to, and caused by asthma, but they are uniquely separate medical entities. One of them I have control over, the other I don’t . Let’s break these components down;
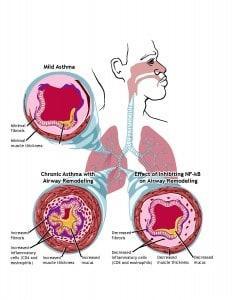
The first and primary component of my asthma, is pretty much the same one that all asthmatics have to some degree, and that is, hypersensitive, mucus producing-inflamed airways. When you have an asthma flare up, it’s the swelling of the lining of the airways, and/or the excessive mucus production, and/or the tightening of the muscle bands that attach to the outside of the airway, and/or ALL all of the above, that causes you to wheeze and feel short of breath. No one really knows why this happens, but luckily, most of these symptoms are treatable, and even preventable, when following an asthma action plan and taking the proper asthma medications. So, as with most asthmatics, this is the part of my asthma that I some control over.
In addition to having sensitive and inflamed airways however , I also have a 2nd component often seen in severe asthmatics. This involves the scarring and/or the loss of what they call “alveolar attachments” (essentially, elastic fibers which help pull the alveoli open from the outside).
Years and years of unchecked asthma exacerbations and multiple intubations, has caused structural changes to occur within my airways (what they call remodeling). The tissue that lines the inside of my breathing passages is literally scarred over, causing permanent narrowing ( see illustration above). Scarring of the airways looks just the way you would imagine any scar tissue to look. It’s thick, fibrous and pale looking. ( Click here to view the inside of my actual airways). Because of this scarring, my lung function and expiratory flow rates(Spirometry) are severely diminished. The combination of a loss of elastic recoil and a loss of alveolar attachments, makes it hard for me to empty my lungs completely (air trapping), which results in chronic breathlessness, sometimes severe.
It’s unknown whether airway remodeling is reversible, but the scarring component probably is not. Hence, this is the part of my asthma that I cannot control. Short of lung transplant, there’s not really a lot that can be done for me. All I can do is try and prevent the deterioration from getting worse. Ironically, it’s thought by some asthma researchers, that this kind of scarring might actually have a protective effect on the weaker airways and alveoli by preventing them from collapsing in on themselves. This might explain why Ive been able to bounce back so quickly from some really severe exacerbations.
The inside of my air passages are so narrowed that even the slightest bronchospasm or inflammation in those airways can cause them to completely close up. And unlike people with”regular” asthma, my lung function is so low to begin that I have no reserve to fall back on when I start to flare, which is probably why I get so sick.
The message here is simple, if you wanna maintain some control over your asthma, take your disease seriously from day one. Take your medications as prescribed and do everything you can to keep your symptoms in check, so that you can minimize your chances of developing “Double Whammy” asthma. If you find that you’re unable to control your symptoms, try to get evaluated by a Pulmonologist who specializes in severe asthma . I can’t tell you how many general practitioners Ive seen over the years who claimed they knew everything there was to know about treating asthma , but obviously didn’t ( but that’s another post).
Addendum : As of 2013 there’s actually a medical term for “double whammy asthma”, they call it ACOS or Asthma COPD Overlap Syndrome. I believe you’ll be hearing more about this in the near future. Also, there is now a phenotype to describe my asthma..”TH2 low, Mast cell high with remodeling”
There’s also a small glimmer of hope now that at least some forms of severe asthma might actually be treatable someday. The key, is asthma research and finding out why scarring or remodeling occurs in some asthmatics and not in others. This is why the the work of people like Dr Sally Wenzel is so crucial.



My father is a 71 year old male who has been on every asthma treatment around and as many have found only steroids have been effective. He has been on prednisone (sp) for the better part of 20 years. He is at the point where he has to sleep sitting up with CPAP machine mask on. The doctor says that his oxygen levels in his blood are such that they cannot prescribe O2. Has anyone heard of this anyone have suggestions? I would like to make him comfortable he has been to every doctor and specialist on the planet and the best hospitals in NYC. Something that can give him hope would be great. His heart is in good shape surprisingly his liver is in good shape. Blood pressure has been good. My father is a veteran with purple heart to show I say this because maybe there is something out there for aging verterans pleases advise. Thank you for reading.
Dale
Hello, Sorry to hear about your Dad, I can certainly relate.
I’ll be honest with you, it’s difficult for me to make any suggestions without actually reviewing medical records and talking with the person. I will tell you however, that it’s not uncommon for people with severe chronic asthma , not to require supplemental oxygen. Unlike emphysema, asthma or asthma/COPD overlap disease effects the airways, not the alveoli where gas exchange takes place.
I know you mentioned that you’ve seen tons of medical experts, but because your father has been on steroids so long, you might want to try to get a hold of Dr Wenzel at the University of Pittsburgh for an evaluation. She deals almost exclusively with life long steroid dependent asthmatics and is one of the best asthma doctors in the world. You can find her contact info on my blog or I can provide it to you.
I wish I could offer more help. You’re Dad obviously has a very caring Son.
Steve
Hi. Good morning! I am posting a comment about my having contracted adult asthma after my having undergone open major surgery for the removal of my oesophagus, I had a 5cm cancerous tumour at the base of my oesophagus.
Whilst undergoing the surgery I had been informed by my consultant that my right lung would need to be deflated, in order to enable access to my oesophagus. Unfortunately, whilst my right lung was indeed deflated, my left lung was “inadvertently nicked.”
I subsequently spent 3 weeks in the ICU, being ventilated and a further 3 weeks in a general surgery ward where I had to be taught to both walk and talk again. This has left me probe to ongoing serious lung infections and I also have been prescribed 2 asthma inhalers.
This has been going on nie for 2 years and I am really worried about my longer term prognosis, I am 63 years old. Coujd you please advise, comment on my present condition and if appropriate, please advise me on the treatments that I should access. Thank you ??
Michaelmcgeown
Im very sorry to hear about the problems you’ve been having since your surgery. Im afraid I can’t offer much advise, as my specialty is asthma, not cancer. Did you have asthma or COPD prior to your surgery? All of these conditions and the use of oral or inhaled steroids can make you more prone to lung infections.
I hope you find some answers.
Xx Steve